Gastrointestinal Cancer
Your Trusted Partner in Gastrointestinal Cancer Treatment

Advanced Head & Neck Cancer Treatment You Can Trust
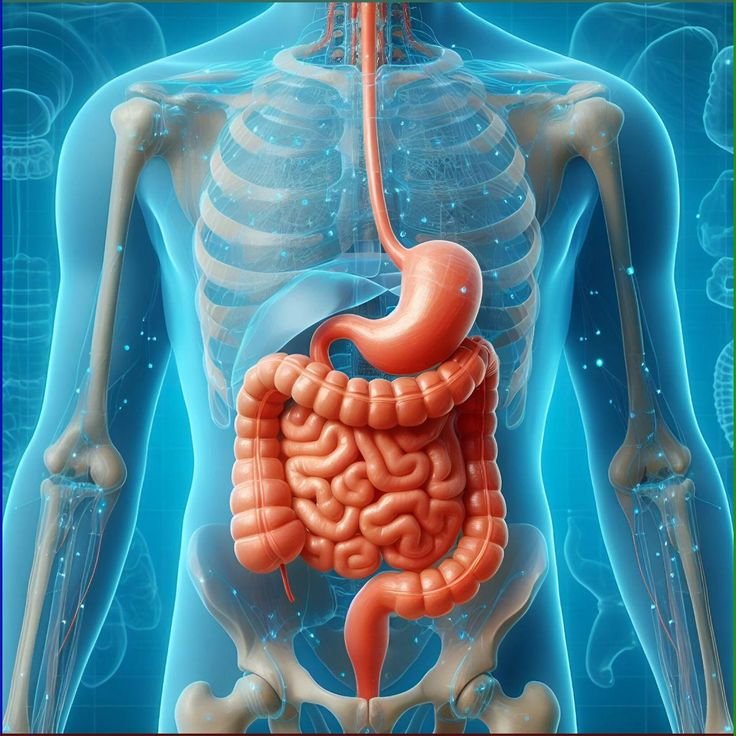
Gastrointestinal (GI) cancer is a term used for cancers that develop in the digestive system, which includes the esophagus, stomach, liver, pancreas, gallbladder, colon, and rectum. These cancers often grow silently, and early symptoms may resemble common digestive problems such as indigestion, bloating, or changes in bowel habits, which makes timely diagnosis challenging. As the disease progresses, patients may experience persistent abdominal pain, difficulty swallowing, unexplained weight loss, fatigue, or blood in stool. Because the digestive system is vital for overall health and nutrition, GI cancers can have a significant impact on a patient’s well-being if not detected and treated early.
Diagnosis typically involves advanced tests such as endoscopy, colonoscopy, CT scans, MRI, PET scans, ultrasound, and biopsies to confirm the type and stage of cancer. Blood tests and tumor markers may also be used to guide treatment. Once diagnosed, treatment is personalized according to the type of cancer, its stage, and the patient’s overall health. Surgery is one of the most common approaches to remove tumors, often combined with chemotherapy and radiation therapy to ensure cancer cells are destroyed. In advanced cases, newer options like targeted therapy and immunotherapy are increasingly used, offering more precise and effective treatment with fewer side effects.
Causes & Risk Factors
- Genetic mutations and family history of GI cancers
- Unhealthy diet (high in red/processed meat, low in fiber, fruits, and vegetables)
- Smoking and excessive alcohol consumption
- Obesity and lack of physical activity
- Hepatitis B or C infection (linked to liver cancer)
Signs & Symptoms
- Persistent abdominal pain, bloating, or discomfort
- Indigestion, nausea, or frequent vomiting
- Difficulty swallowing (especially in esophageal or stomach cancer)
- Changes in bowel habits – diarrhea, constipation, or narrowing of stool
- Blood in stool or black, tarry stools

Life After Treatment
Life after treatment for gastrointestinal cancer is a journey of healing, adjustment, and ongoing care. Many patients may notice changes in digestion, energy levels, or appetite, but with proper guidance these challenges can be managed effectively. Nutrition plays a vital role in recovery, and working with a dietitian helps patients adapt to new dietary needs while maintaining strength. Regular physical activity, even light exercises, can restore stamina and improve overall well-being.
Prevention & Awareness
- Eat a balanced diet rich in fruits, vegetables, whole grains, and fiber
- Limit consumption of red and processed meats
- Maintain a healthy body weight and stay physically active
- Avoid smoking and limit alcohol intake
- Manage chronic digestive conditions like GERD or IBD under medical supervision
Treatment Options
We provide a wide range of treatments tailored to each patient’s specific condition
Surgery
Removal of cancerous tumors with reconstructive surgery when needed.
Radiation Therapy
High-energy rays used to target and kill cancer cells.
Chemotherapy
Medications that destroy or shrink tumors, often combined with radiation.
Targeted Therapy
Precision medicines that attack specific cancer cell proteins.
Immunotherapy
Boosts the body’s natural defenses to fight cancer.
Rehabilitation
Speech therapy, swallowing therapy, nutritional support, and psychological counseling to help patients recover fully.
FAQ
Frequently Asked Questions
What is gastrointestinal (GI) cancer?
Gastrointestinal cancer refers to cancers that develop in the digestive system, including the esophagus, stomach, liver, pancreas, gallbladder, colon, and rectum.
What causes GI cancer?
There is no single cause, but risk factors include unhealthy diet, smoking, alcohol use, obesity, chronic digestive diseases, infections like H. pylori or hepatitis, and family history of cancer.
What are the early signs of GI cancer?
Early symptoms may include indigestion, abdominal discomfort, bloating, changes in bowel habits, unexplained weight loss, or fatigue. However, some GI cancers may not show symptoms until later stages.
How is GI cancer diagnosed?
Diagnosis may involve endoscopy, colonoscopy, imaging tests (CT, MRI, PET scans), blood tests, and biopsy to confirm the type and stage of cancer.


